Caregiving has an impact on caregivers’ health. We examined the effect that support policies for caregivers have on their health, and results revealed that non-financial support policies have a larger protective effect than financial ones. Specifically, the policies showing a stronger association with a better health were those providing caregivers with free time, helping them to deal emotionally with caregiving, and giving them skills to improve the care situation.
The article “What seems to matter in public policy and the health of informal caregivers? A cross-sectional study in 12 European countries” published in PLOS One examined the effect that support policies for caregivers have on their health. We used SHARE data from 13,502 caregivers from 12 European countries.
With the ageing of the population, and in times of welfare state retrenchments and cutbacks, informal caregivers are one of the most important assets to ensure that care is provided to the growing population in need of care. Evidence shows that caregiving has an impact on caregivers’ health. Thus, support measures are necessary to keep caregivers in good health, so that the informal caregiving system is maintained. However, there is little information on how do these support measures impact the health of informal caregivers.
Caregiving impact on health is mediated by many determinants, such as caregiver’s skills or personality. Caregiving is also shaped by the social context of each country, and for example, in generous welfare states caregiving is mainly provided by professionals, while in less developed welfare states the family is required to provide most of the required care. Moreover, across the globe, caregivers are predominantly women, which may be a source of health inequalities. However, men are assuming increasingly important roles as caregivers due to changes in population demographics.
Our results indicated that as expected, support measures moderate the health of caregivers. However, while non-financial support measures such as training, education, respite care and counseling seemed to be strongly associated to an improved health of the caregivers, financial support measures had almost no association. This lack of efficacy of financial support measures may be explained by the fact that, in general, financial support measures are earmarked for the care recipient and not for the caregiver since for example, a caregiver allowance is available only in 4 of the 12 countries included in our study.
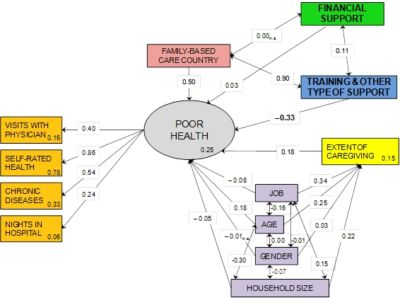
Figure: Path analysis showing the association of caregiver’s health with the diverse policies of support to caregivers (n.s.= non-significant, p≥0.05; Values within the boxes are r2 values).]
We found that the poorest health was reported by those giving care inside their households, which may be due to the fact of being emotionally closer to the recipient of care and to the fact that they cannot evade the care situation easily as those giving care outside their household. The health of caregivers is also affected by the family relationship with the cared-for person (spouse, parent…), and, although we lack this information, we know that those giving care inside their households are older than those giving care outside, so it could also be that caregivers with worse health choose (or can only) give care inside their household, and that younger and healthier individuals can give care outside.
We also analyzed the effects of living in a family-based country or not. That is, of living in countries where the family is the main supplier of care. We saw that living in a family-based country has a significant effect on the health of caregivers, which may be due to the fact that living in a family-based country may lead many people –who may already have bad health- to provide care to relatives just because this is the role they are expected to play.
Regarding gender differences, in our study there were more women than men caregivers. However, we detected no specific gender differences in our sample.
In sum, our study shows that non-financial support measures (education, training, respite care, non-paid leave and counseling) seem to have a larger protective impact on caregiver’s health than do financial support measures. However, further longitudinal studies to establish causal effects are warranted.
About the author(s):

Dr. Laia Calvó-Perxas, IDIBGI Girona Biomedical Research Institute, Girona IDIBGI
The article is based on:
Calvó-Perxas, L., J. Vilalta-Franch, H. Litwin, O. Turró-Garriga, P. Mira and J. Garre-Olmo (2018). What Seems to Matter in Public Policy and the Health of Informal Caregivers? A Cross-Sectional Study in 12 European Countries. PLOS One. https://doi.org/10.1371/journal.pone.0194232.










Leave A Comment